
(AFP Photo / Noel Celis)
As Egypt records one of the highest infection rates of Hepatitis C worldwide, hundreds of thousands of patients, especially those who have reached end stage liver disease, struggle due to liver failure. Only a lucky few manage to recoup their health and independence through a liver transplant. It is not easy. A typical Hepatitis C patient undertakes a long journey before finally locating an eligible donor who consents to donate more than half of his or her healthy liver.
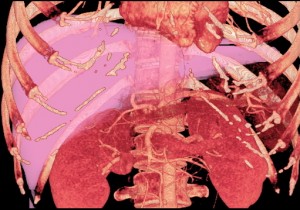
Scientifically, end-stage Hepatitis C entails the destruction of the liver, which is severely affected by the Hepatitis C virus. The virus is stealthy, and once contracted, can silently damage the liver enzymes for over twenty years without the patient becoming aware of the problem. Eventually, the disease may progress to cause fibrosis of the liver. In some cases, if the liver is less severely damaged, a drug called interferon may be able to halt the disease by suppressing the active virus. Interferon is a long-term treatment and does not usually lead to the total eradication of the virus. Therefore, liver transplants, entailing the replacement of the diseased liver with all or part of a healthy one, are the most effective solution for Hepatitis C sufferers.
According to ‘Hepatitis C: The cure’, an article published in March 2013 by the Financial Times magazine, the virus has always been elusive and difficult to treat. “No one knows how the virus got started: maybe in dogs, or bats. Different variations, known as genotypes, exist in different parts of the world. It has certainly existed for thousands of years, but because the virus travels in the blood, for centuries it never moved very far,” reads the article. For more than 20 years, the virus was known merely to be a type of hepatitis, denoting an inflammation of the liver, and was described as “non-A, non-B hepatitis”. Scientists and liver specialists are currently debating the effects and use of Sofosbuvir, a newly-developed drug that scientists hope will be a breakthrough treatment for Hepatitis C. A week ago, news was released that Sofosbuvir had improved the cure rate of two subtypes of Hepatitis C, according to the UPI.com health journal.

(AFP Photo)
Samaah’s story
In many poor neighbourhoods across Cairo, millions of Egypt’s citizens struggle to survive. Illiterate, desperate, and hungry, many choose to undergo liver transplants as donors in return for large sums of money. Samaah is one of those.
“My husband is a drug addict. I don’t depend on him to provide for our kids or me financially. But, I needed the money urgently to help my daughter get married,” says Samaah, who donated 60 per cent of her liver to a Hepatitis C sufferer for EGP 50,000. Lying in her bed after undergoing almost 10 consecutive hours of invasive surgery, the 37-year-old cleaning lady at a school says she is totally convinced that her decision to donate a large section of her liver to another patient was a good one. “I am happy I did that, and I knew it was very risky and could lead me to serious health problems,” she says. Only recently did it cross Samaah’s mind that she could quickly earn EGP 50,000 in return for 60 per cent of her liver. Samaah’s story started when she heard of a Hepatitis C patient asking around for an eligible donor. At a private school in the Cairo neighbourhood of Haddaiyeq Al-Qubba, the donor chatted with a common friend about her decision to give away part of her healthy liver to save another Egyptian.
“I was sitting with one of my colleagues at work when she told me that there was a teacher who was suffering from end-stage liver disease and was offering a lot of money to an eligible liver donor,” she explains. Living with her two sons and soon to be married daughter, Samaah states that her dire need for money was the main factor behind agreeing to undergo the liver transplant surgery. “I honestly knew it was dangerous for me, but I decided to undergo the operation and I only told my husband and sister about it. None of my kids know that I have donated a big part of my liver,” she says.

(AFP Photo)
The donation
Dr. Wahid Doss, Dean of the National Liver Institute, explains that before proceeding with any liver transplant surgery doctors usually sit with the donor and explain to him/her all the possible side effects that could result from the operation. These can include pneumonia, blood clots on the lungs, temporary liver failure, and even death. “The donor listens carefully to all the side effects and has to sign many consent forms stating that he/she fully understands and agrees to the procedure,” says Doss. He adds that although Samaah was firmly convinced to undergo the procedure from the very beginning, many donors change their minds after reflecting on the possible post-surgery side effects of the transplant. “For some people, it is all about the money,” Doss explains.
Samaah, who used to weigh 94 kilos, had to lose more than 20 kilos in three months in order to be able to donate part of her healthy liver. “Three months before the surgery, I had follow-up meetings with the doctors and I underwent various blood tests, liver enzymes tests and many other scans. I was told that I had to lose a lot of weight before the liver transplant,” she says.
Explaining the exact procedures of a liver transplant, Doss states that a Hepatitis C patient seeking a transplant is usually faced with two problems. The first is to be able to find an eligible donor; the second is to be financially able to afford the liver transplant surgery. The cost of typical liver transplant surgeries in Egypt ranges from EGP 200,000 to EGP 400,000 including the hospital expenses. The first step taken after a patient finds a donor is to present all his documents and test results to an ethical committee, usually found at any hospital, to study the case. “Liver transplants have a humanitarian aspect. If the donor is not a relative, the committee needs to assess whether or not he/she is supplying the biggest part of his/her liver without any pressure from anyone,” Doss says, elaborating that in some cases “coercion” from families and friends can take place. The committee then transfers the file to the High Committee of Organ Transplant, which belongs to the Ministry of Health, to give the case final approval. The High Committee of Organ Transplant was established in Egypt due to Law 5, which was passed in 2010, and exists to regulate all organ transplants across the country.
According to Doss, Egyptian law rules that a donor may be any of the patient’s relatives who is between the ages of 20 and 40 and is free of any diseases. He points out that only about 22 hospitals in Egypt perform liver transplants, including educational hospital universities, military hospitals and a small number of private hospitals. In 2012, the country finally issued a law that sets the rules for general organ transplant.
Meeting the legal conditions to become an eligible donor is not easy. The husband of the Hepatitis C sufferer to whom Samaah donated part of her liver speaks about how difficult it was to find an eligible donor. “After finding out that my wife was suffering from end-stage liver disease, we kept asking around everywhere for an eligible donor. Nobody was suitable in her case. Many donors accept a deposit of EGP 5,000 and then flee away,” he says. Doss says he hears of hundreds of cases of intended donors who take the money but simply disappear as little as one hour before the surgery takes place. “There is a lot of trickery and many con-artists in the liver transplant process,” the patient’s husband, who preferred to remain anonymous, says. Before Samaah came on the scene, he explained, the family struggled to find an appropriate donor to save his wife’s life.
(Photo from Taichung Veterans General Hospital)
Role of the broker
A broker, who mediates between donors and patients, says he usually receives about 10 per cent of the total cost of the surgery. “I help Hepatitis C patients find a relevant donor. If we agree on the price of the donation I begin to search for an eligible donor,” he says. The broker, who refuses to give his name, explains that there are many others who earn money from the liver transplant business. “I work closely with doctors who treat Hepatitis C and I have been working in this business for about seven years,” he says. When the broker brings in a potential donor, he receives around EGP 10,000 and the donor takes about EGP 5,000 until he or she passes all the requested blood tests. “If the tests prove he or she can medically proceed with the surgery, I take another EGP 5,000 after the completion of the surgery,” the broker says.
But the patient’s husband says that they tried to approach several liver brokers. Two brokers took deposits for their services, promising to find the couple an eligible donor, but then disappeared. “Some brokers are thieves. It was only thanks to good luck that we managed to get in contact with Samaah,” he says.
Doss elaborates that the donor should be a close relative of the patient and has to have the same blood group as the patient, a liver which is large and healthy enough to donate a piece, and should be free from any diseases with good results in all liver function tests. If the donor is not a relative, doctors need to apply the same criteria if they are considering a foreign donor and also make sure he or she understands the risks he or she is putting him or herself through. The transplant operation usually lasts from 8 to 12 consecutive hours.
“I knew it was going to last for many hours. I stayed in surgery for about 8 hours and then I got out. The patient receiving part of my liver stayed in surgery for another five hours,” Samaah says.
Rise in surgeries
Since 2001, around 2,000 liver transplant surgeries have been conducted for Hepatitis C patients. Gamal Heshmat, a professor of liver diseases at Qasr El-Einy hospital, says that during 2012 alone Egyptian doctors performed 300 to 400 liver transplant operations. He adds that there are about 150,000 Hepatitis C sufferers in Egypt, and about 15,000 of them are experiencing end-stage liver failure and require liver transplants immediately.
“The problem lies not only in the high number of the patients already diagnosed with Hepatitis C, but also in the growing number of people who are infected every year by the same virus,” Heshmat says. He explains that every year about 15,000 people discover that they are carrying the virus, which is transferred through the blood in procedures like blood transfusions or the use of unsterilised medical equipment. “Most of the infections occur inside medical institutions, in hospitals, clinics or other medical centres in Egypt,” the liver specialist says.
In October 2012, the National Committee for the Control of Viral Hepatitis established the country’s first Hepatitis C patient registry. This has helped many patients to connect with others who have been treated with Interferon to combat the virus. This registry has helped to assess the extent of many other related issues to the virus, analyse new data and recognise the most common methods of infection.
“I will get out of the hospital tomorrow morning. After the surgery was finished, I received the rest of the money that we agreed on before the surgery. I actually think it was great that I managed to save a person’s life and at the same time managed to earn a lot of money very quickly,” Samaah says, adding that she will start preparing for her daughter’s wedding as soon as she recuperates.




